Respiratory Conditions that Require Bronchoscopy
What is Bronchoscopy?
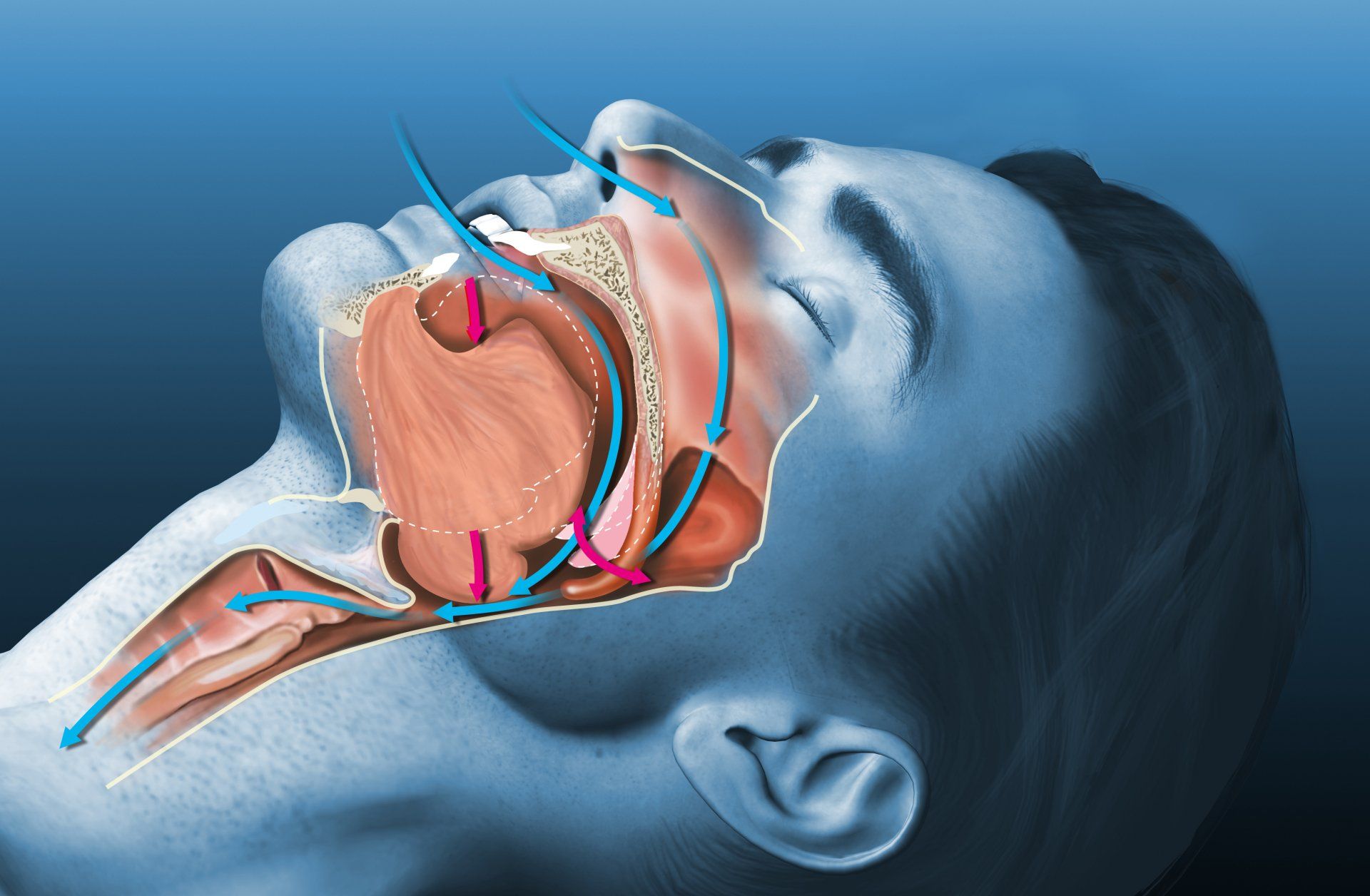
A bronchoscopy is a procedure whereby a narrow tube (bronchoscope) with a camera at its end is inserted through your mouth or nose, down your throat, in order to look inside your airways. Bronchoscopes may be flexible or rigid. Most bronchoscopy procedures are done with flexible bronchoscopes.
What conditions would require bronchoscopy?
Conditions that may require bronchoscopy can be divided into conditions arising from the:
Airway
Tumours
Hemoptysis (coughing of blood)
Secretions (phlegm)
Narrowed areas in airways (strictures)
Lung Tissue and Nearby Structures
Tumours
Infection or inflammation
Intersitital lung disease
Lymph node enlargement
Why is bronchoscopy needed for each of these conditions?
For most cases of flexible bronchoscopy, this investigation is meant to find out the cause of the lung condition that had been detected through symptoms and radiologic imaging (chest X-ray or computed tomography (CT) scan of the chest). During the bronchoscopy, a biopsy or lavage (the collection of your secretions) can be done in order to diagnose lung disease or cancer. A more advanced investigation is endobronchial ultrasound-guided transbronchial needle aspirate (EBUS-TBNA). This employs a bronchoscope with an attached ultrasound probe that allows the specialist to see structures outside the airway, such as enlarged lymph nodes, which can arise from conditions such as cancer or inflammation.
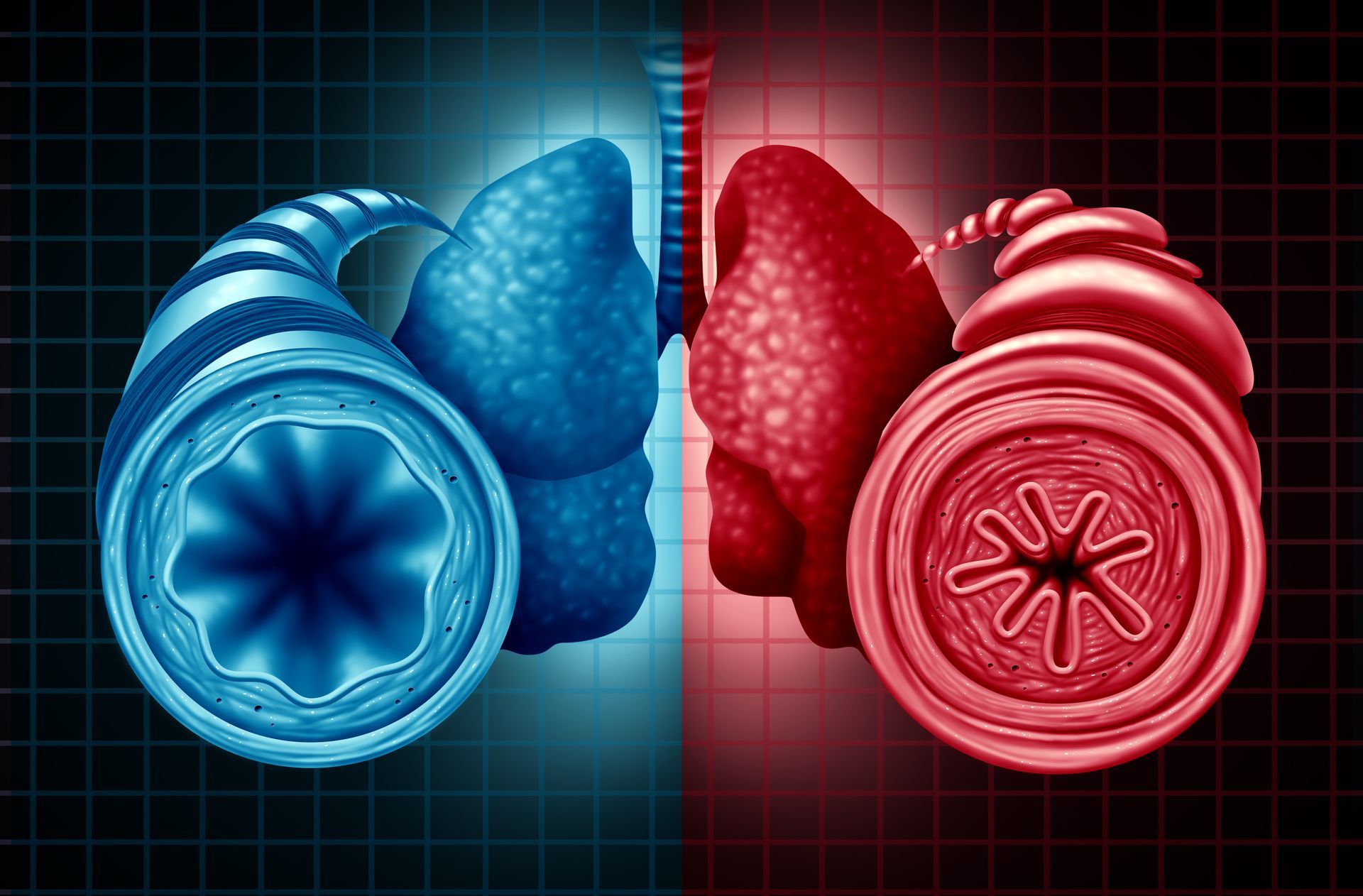
In some conditions such as severe asthma, flexible bronchoscopy may be a form of treatment. This is known as bronchial thermoplasty, where controlled heat energy is delivered to the smooth muscles of the asthmatic airways, leading to a reduction in the amount of excessive smooth muscle. With less smooth muscle, the airways constrict less during an asthma attack, making breathing easier.
What should the patient expect before, during and after the bronchoscopy procedure?
Before bronchoscopy
Before performing a bronchoscopy, your lung specialist will talk to you about the intentions of the procedure, the risks involved and what he may expect to find. You will be asked to sign a consent form. If you are on any blood-thinning medications, such as aspirin, clopidogrel (Plavix) or warfarin (Coumadin), you may be asked to discontinue these for a period of time before the test. In addition, you will be asked to fast (not eating or drinking) for 4-6 hours before the bronchoscopy.
During bronchoscopy
At the start of the bronchoscopy, you will be given a local anaesthetic to numb your throat and nose, followed by a sedative medication to make you sleepy. The duration of the bronchoscopy can vary, anywhere from 10 minutes to 1 hour, depending on what the specialist sees during the procedure and what needs to be done, e.g. biopsy. Throughout the procedure, your blood pressure, heart rate and oxygen level will be continuously monitored.
After bronchoscopy
After the bronchoscopy, you will be monitored for 2-4 hours in the recovery area. You may continue to feel groggy because of the sedatives administered to you. As the effects of the medications can last for several hours, it is important that you are accompanied by someone who will be able to take you home. Typically, you are able to eat and drink after 2-3 hours. You will experience some throat irritation and may cough up small amounts of stale blood for a day or two after the bronchoscopy- this will recover naturally. Your lung specialist will also review the outcome of the bronchoscopy (such as lavage and/or biopsy results) which will be available a few days after the procedure.
Respiratory Medical Associates is an established specialist group that is recognised as one of Singapore’s leading experts in bronchoscopy. The group is well versed in bronchoscopic techniques such as bronchoalveolar lavage, transbronchial lung biopsy, ultrasound-guided transbronchial needle aspiration of mediastinal lymph nodes and bronchial thermoplasty.
Enquire now at
info@respmed-associates.sg/ For further reference, please refer to:
https://www.respmed-associates.sg/bronchoscopy