Respiratory Patient Care: Introduction to Bronchoscopy
What is bronchoscopy?
A
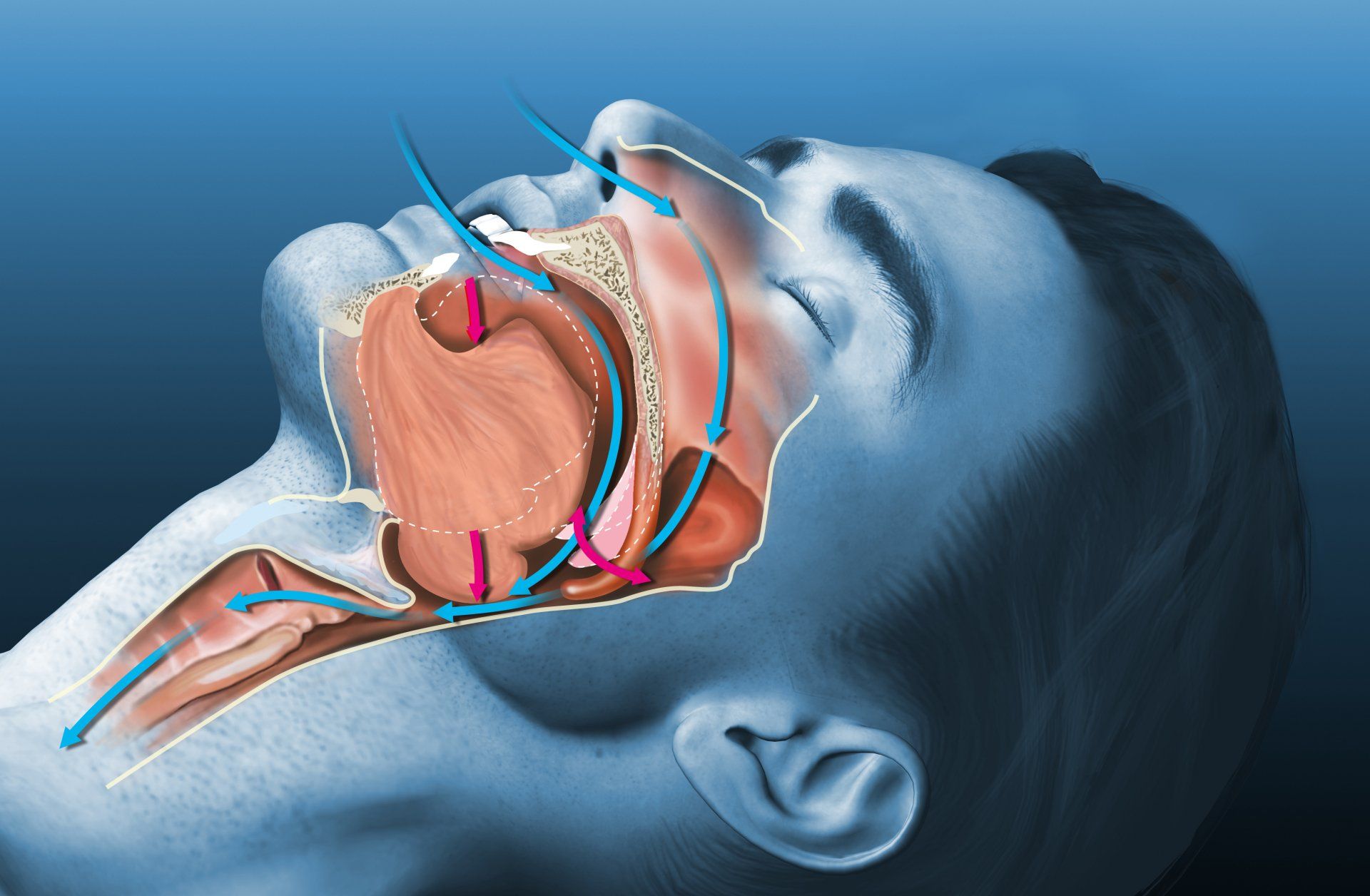
bronchoscopy is a procedure whereby a flexible, narrow tube with a video camera attached to one end (bronchoscope) is inserted through your mouth or nose in order to look inside your airways. It is usually done using conscious sedation i.e. you will be given a medication to make you sleepy.
When would you undergo bronchoscopy?
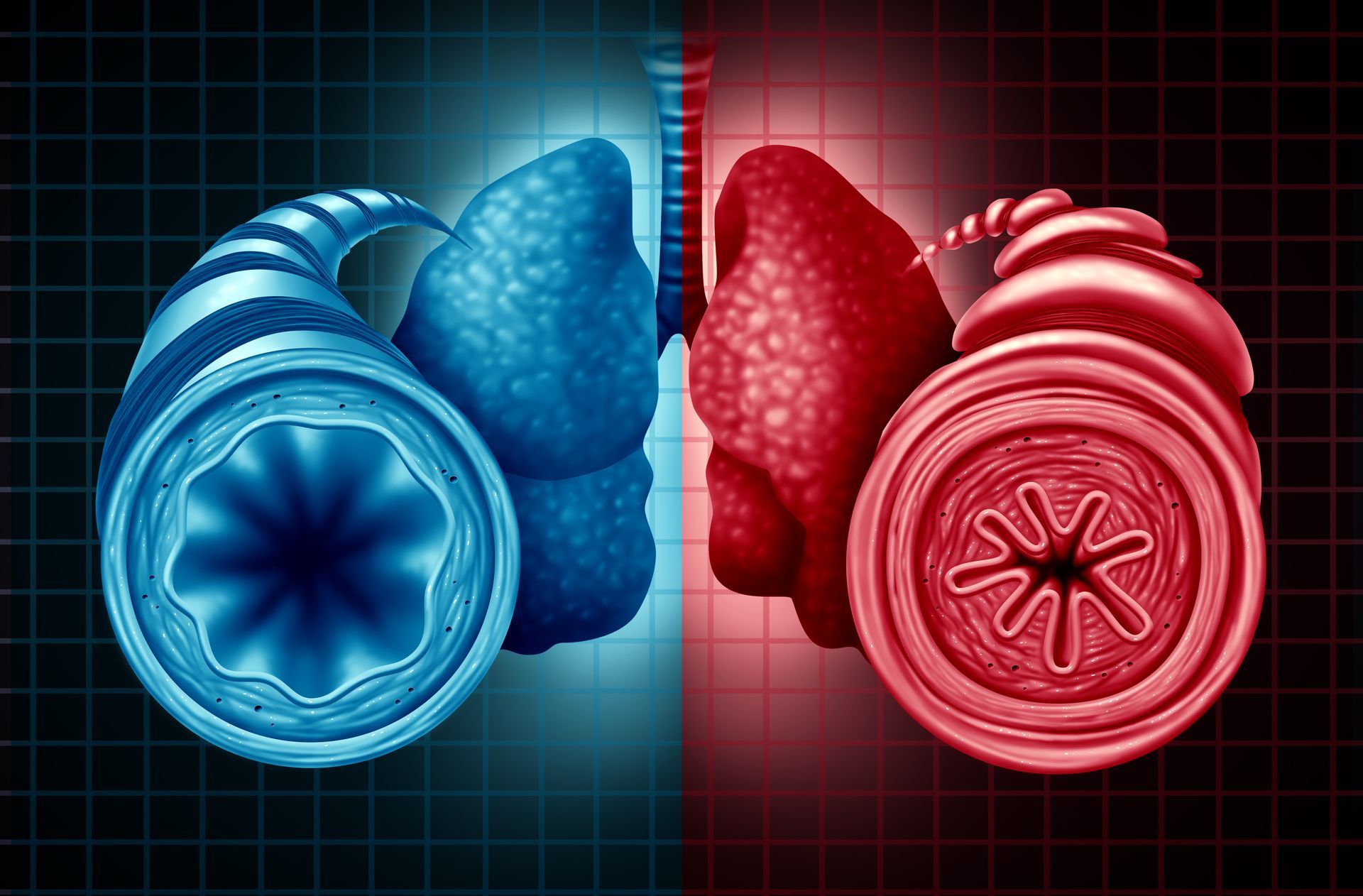
Bronchoscopy is used to evaluate lung symptoms such as chronic cough, coughing of blood or when lung disease or cancer is suspected after X-ray or CT studies. During bronchoscopy, doctors are able to see the inside of your airways. If there are areas that are abnormal, a biopsy (tissue sample) or lavage (washing the airways and collection of your airway secretions) can be done in order to diagnose lung disease or cancer and guide subsequent treatment. In addition, bronchoscopy may also be used for treatment e.g. to temporarily stop bleeding in the airways or in the case of airway narrowing, to insert a stent to open up the airway.
Things to Keep in mind before during and after the procedure
Before the procedure, your specialist will assess your suitability for bronchoscopy. Your specialist may advise you to stop certain medications, such as those that thin your blood (for example aspirin, clopidogrel, anti-coagulants). You will be required to fast for about 6 hours prior to bronchoscopy.
During the procedure, everything will be done to ensure your comfort. A local anaesthetic will be applied to your nose and/or the back of your throat to numb the area so that you are less likely to gag when the endoscope is introduced. Once you have been sedated, the bronchoscope will be gently introduced through either your mouth or nose. You will be able to breathe easily throughout and you will be given additional oxygen supplementation. Your vital signs (pulse, blood pressure and oxygen level) will be monitored regularly throughout the procedure. The bronchoscopy usually takes about 15 – 45 minutes, excluding preparation time. Depending on your lung condition, it may be necessary to obtain a lavage or a biopsy. A biopsy can be performed by using a hollow needle or with a pair of small forceps. X-rays or ultrasound may be used to guide the biopsy.
After the bronchoscopy, you will be monitored for 2-4 hours in the recovery area. Your throat may feel mildly sore and you may continue to feel groggy because of the sedatives administered to you. Typically, you are only able to eat and drink after 2-3 hours. You may cough up small amounts of stale blood for a day or two- this will usually resolve with time. As the effects of the sedation medications can last for several hours, you are advised to be accompanied by someone who will be able to take you home.
What are the complications and risks of bronchoscopy?
Bronchoscopy is usually very well-tolerated. Occasionally, the following complications may occur:
- Coughing, throat soreness and/or voice hoarseness can occur after bronchoscopy. This will usually resolve naturally 1 – 2 days after the bronchoscopy.
- Fever. This may happen after lung washings are done and is treated with paracetamol.
- Complications related to the sedative medications, such as slowing of breathing, reduction of oxygen levels in blood and lowering of blood pressure during the bronchoscopy. This is minimised by administering appropriate amounts of medication before and during the procedure, as well as monitoring of your vital signs during and after the procedure.
- Low oxygen levels. During the procedure, your oxygen levels are measured and you will be given additional oxygen supplementation as required.
- Bleeding can occur after biopsies. Normally it is only minor and settles quickly. If necessary, the lung specialist will give medications via the scope to help the bleeding stop.
- Pneumothorax (collapse of the lung due to a collection of air trapped in the cavity between the lung and the chest wall) can occasionally occur, especially after a biopsy. Pneumothorax can recover by itself, but for some patients, a tube has to be inserted through the chest to remove the air from around the collapsed lung. This may prolong your hospital stay.
- Heart complications such as an abnormal rhythm or even a heart attack can rarely occur. Your heart rhythm will be monitored continuously during the procedure.
Is bronchoscopy required for your lung condition? Get a specialist consultation at Respiratory Medical Associates
Respiratory Medical Associates is an established specialist group that is recognised as one of Singapore's leading experts in the diagnosis and treatment of lung disorders. Our specialists are trained in advanced bronchoscopic techniques, such as bronchoalveolar lavage, transbronchial lung biopsy, endobronchial ultrasound and bronchial thermoplasty. Enquire now.