Pneumonia In The ICU - What To Expect
Suppose your loved one has been sent to the intensive care unit (ICU) of a hospital. In that case, it indicates that their condition is critical enough to require the highest level of medical care and the most rigorous measure of medical monitoring. On the other hand, having a loved one sent to the ICU due to respiratory-related issues, such as pneumonia, can be even more distressing to the patient’s loved ones because it also means that the patient is struggling to breathe.
However, with highly trained specialists, the ICU aims to provide treatment, supervision, and assistance to patients with severe pneumonia. So, let's take a closer look at what to expect when someone you know is in the ICU for pneumonia.
Overview
The ICU differs from other hospital wards in the following ways:
- A group of specialists, including nurses, medical assistants, therapists, etc., who are highly qualified to conduct their jobs will provide care and supervision around the clock.
- The number of beds is smaller, but the medical team monitoring and caring for the patients is much larger.
- Visits are more strictly regulated.
On the other hand, the ICU for respiratory issues is a facility that offers close supervision and intensive therapy to patients who have acute or severe respiratory failure caused by a respiratory illness.
Some conditions that require careful monitoring include the following:
- Severe COVID
- Acute Respiratory Distress Syndrome
- Acute or chronic respiratory failure
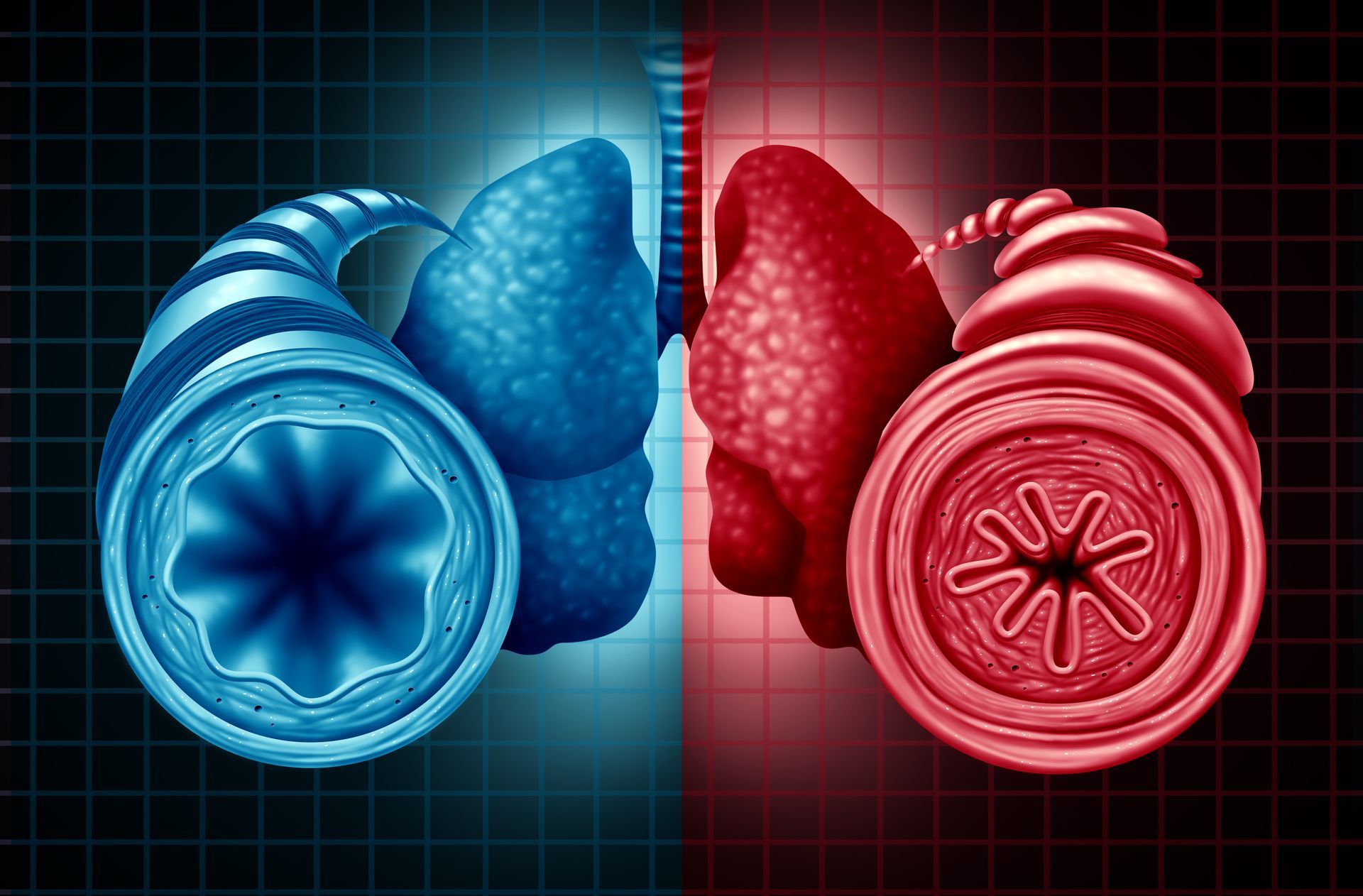
- Chronic Obstructive Pulmonary Disease (COPD)
- Chronic bronchitis
What is pneumonia?
Pneumonia is an illness that causes the air sacs in one or both lungs to become inflamed. The air sacs may swell with fluid or pus, resulting in the following:
- cough that produces pus or phlegm
- fever
- chills
- breathing difficulties
Pneumonia can be brought on by a variety of organisms including:
- bacteria
- viruses
- fungus
When intensive care is needed during pneumonia
An individual that is suffering with severe pneumonia will be sent to the ICU. The symptoms of severe pneumonia includes:
- Risk of heart, kidney or circulatory system failing
- The lungs can no longer take in oxygen
In most cases, an antibiotic infusion in intensive care is required, along with artificial breathing or other medications such as corticosteroids.
What intensive care equipment is needed for Pneumonia
The stabilisation of your loved one is crucial if they are admitted to intensive care for the treatment of pneumonia since they typically have subsequent respiratory failure. Here are some of the equipments that will be used during their time in the ICU include:
Bedside Monitors
When a patient is in an ICU, the bedside monitors are used by the specialists to monitor the essential body funtions.The main bodily functions are shown on the ICU monitor, which resembles a television or computer screen. Most often observed bodily activities include:
- Blood pressure
- Breathing rate
- Oxygen saturation
- Body temperature
- Heart rate and rhythm (ECG)
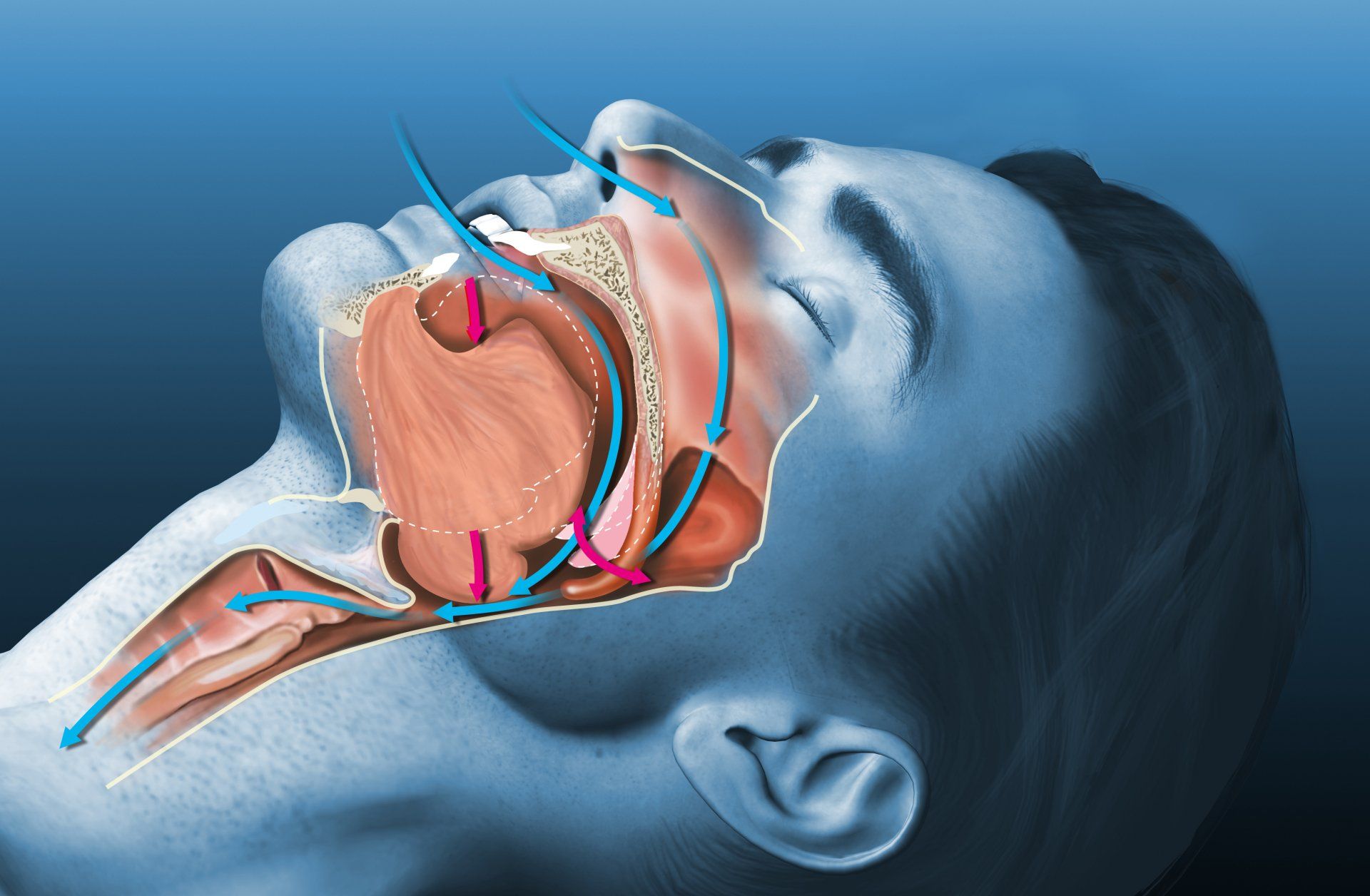
Non- Invasive Ventilation (NIV)
Non-Intrusive Ventilation (NIV) is the use of Ventilators (Breathing Machines) to provide ventilatory support without the need for an invasive artificial airway (Breathing Tube/Endotracheal Tube or Tracheostomy).
Typically, NIV is administered using a (CPAP) mask connected to a circuit, and the circuit (tubing) is connected to the ventilator. NIV ventilation's primary objectives are to increase oxygenation and prevent intubation.
NIV will be administered to ICU patients who are being treated for severe pneumonia to provide sufficient oxygen to the lungs and support the respiratory system.
Nasogastric Tube (NG tube)
The nasogastric tube is used to feed and give medications and other oral substances such as activated charcoal.
A syringe is used to inject substances into the tube, such as medications or small amounts of fluids. In order to provide continuous feeding, the tube is frequently coupled to an electronic pump that can monitor, control, and signal any feeding interruptions.
Patients who are being sedated for pneumonia treatment will require an NG tube until their gastrointestinal tract is functioning normally or until the patient is capable of swallowing.
Urinary Catheter
An internal tube known as a urinary catheter is used to drain and collect urine from the bladder. A catheter is put into your loved one's bladder for a variety of reasons, including:
- To empty the bladder of a critically unwell patient in order to closely monitor kidney function.
- To adjust fluid intake based on urine output.
- One of the primary purposes of urinary catheterization in intensive care is to allow the patient who is unconscious or under sedation to empty their bladder without becoming incontinent (unable to control the flow of urine) and to prevent urine from getting on their skin.
- For an individual whose lower body is paralysed.
- Incontinence (inability to control urine flow).
Due to the immobility of patients suffering from severe pneumonia, a urinary catherer will be essential to help with the ease for emptying the bladder
What To Expect From A ICU
The goal for patients in the ICU is to stop requiring as much respiratory assistance over time. As the patient gains strength, the doctor may transition them from a ventilator to a CPAP machine, then to an oxygen mask or nasal cannula, and finally to independent breathing.
You might notice wires and tubes attached to the individual. Seeing this can be frightening. However, the doctor can better treat the patient with this equipment. The tubes deliver fluids, medications, and air, while the machines that the wires are connected to allow the doctor to monitor vital signs. These includes:
- Temperature
- Blood pressure
- Breathing and pulse rate
Alarms on equipment like ventilators and other devices notify the medical staff of any abrupt changes. The care team may visit and check on an alert even though it is frequently not a cause for concern. You can ask an ICU staff member any questions you may have concerning any alerts.
The ICU team is highly qualified to take care of critically ill patients. They'll make every effort to be of assistance.
Recovering from intensive care
When patients no longer require intensive care, they can be moved to another ward to continue recuperating before eventually going home. Some patients might discharge from the ICU after a few days, while others might need to spend months in the ICU.
Most patients who leave an ICU will make a full recovery. However, persistent issues may occasionally occur, such as:
- Weakness and stiffness
- Fatigue
- Loss of appetite and weight loss
- Sleep problems
- Depression, anxiety or post-traumatic stress disorder (PTSD)
- Problems with mental abilities – for example, not being able to think clearly and being forgetful
These issues may persist for several months. If they continue to concern you or a loved one, seek medical help. Some patients may need ongoing assistance and care (rehabilitation) to recover.
Our Clinic
Respiratory Medical Associates (RMA) is a specialised clinic for the diagnosis and treatment of lung, sleep and allergy disorder. These can include:
- Persistent coughing
- Spots on chest X-ray
- Lung infection (such as bronchitis, pneumonia and tuberculosis)
Additionally, we we provide treatment for long-term conditions, such as:
- Food and drug allergies
- Obstructive sleep apnea
- Lung fibrosis
- Asthma
- Chronic obstructive pulmonary disease
Hence, our team is equipped and trained to provide the following treatments for patients with respiratory issues in the ICU:
- Management of acute respiratory distress syndrome (ARDS)
- Management of sepsis
- Intubation and mechanical ventilation
- Non-invasive ventilation (NIV)
- Inotropic therapy
- Ultrasound-guided central venous catheter insertion
- Intra arterial catheter insertion
- Percutaneous tracheostomy
Our Doctors
Our specialists at RMA have been trained and are highly qualified to treat patients with severe illnesses in the ICU, particularly conditions relating to the respiratory system. In addition, our doctors are also well-versed in various cutting-edge technologies, including:
- Extracorporeal membrane oxygenation (ECMO)
- High-frequency oscillatory ventilation
- Advanced bronchoscopic techniques
- Airway pressure release ventilation
The sights and sounds of the ICU can be frightening. However, the critical care teams meticulously work with patients, their loved ones, and their oncology team to create a mutually agreed-upon plan of care to get the best results.
Looking for lung screening in Singapore? Get specialist care at Respiratory Medical Associates
Respiratory Medical Associates is an established specialist group that is recognised as one of Singapore’s leading experts in the diagnosis and treatment of lung, sleep, and allergy disorders. These can range from persistent coughs, spots on the chest X-ray to lung infections such as bronchitis, pneumonia, and tuberculosis.
In addition, we also treat chronic disorders such as asthma, chronic obstructive pulmonary disease (a lung disease caused by smoking), lung fibrosis, obstructive sleep apnoea, as well as food and drug allergy. https://www.respmed-associates.sg/